Pathologies & solutions
Flat feet, hollow feet, heel spurs, overpronation, supination, diabetes, arthritis, achilles tendonitis
Shoe insoles are particularly suitable for the treatment of these indications. Shoe insoles, also known as orthopedic insoles, are special inserts that are placed in shoes to correct foot alignment, distribute pressure, relieve pain, and improve overall foot function.
1. Corrective insoles
• These insoles are designed to correct foot deformities, such as flat feet (pes planus) or hollow feet (pes cavus).
2. Support insoles
• They provide extra support to specific areas of the foot, such as the arch or heel, to prevent overload.
3. Cushioning insoles
• These insoles provide extra padding to absorb the impact of walking or running, which is especially useful for heel spurs or other painful conditions.
4. Sports insoles
• Designed for sports activities to support the foot and reduce the risk of injury.
5. Diabetic insoles
• Specifically designed for people with diabetes to prevent pressure sores and ulcers by distributing pressure evenly across the foot.
1. Foam
• Soft and conformable, provides comfort and lightweight support.
2. Gel & Absorbent Foams
• Provide excellent cushioning and comfort, especially in the heel region.
3. Leather, Leather-like Materials & Cloth
• Traditional & modern materials that provide breathability and durability.
4. Plastic/Carbon/Graphite
• Used for more supportive and corrective insoles, provides stability and shape retention.
1. Flat feet (pes planus)
• Arch support to promote correct foot positioning.
2. Hollow feet (pes cavus)
• Cushioning and support to reduce pressure on the metatarsal and heel.
3. Heel spurs (plantar fasciitis)
• Cushioning and support of the heel to relieve pain.
4. Overpronation and supination
• Correction of foot position to promote better alignment and movement.
5. Diabetes
• Pressure distribution and protection from pressure sores and ulcers.
6. Arthritis
• Cushioning and support to reduce pressure on painful joints.
7. Achilles tendonitis
• Heel and arch support to reduce stress on the Achilles tendon.
1. Pain Relief
• Reduce pain through better support and pressure distribution.
2. Improved Foot Function
• Promote proper foot position and movement, which can lead to better overall function.
3. Injury Prevention
• Support the foot and can reduce the risk of overuse injuries and misalignment.
4. Comfort
• Provide additional comfort, especially when standing or walking for long periods.
1. Individual fitting
• For the best possible results, shoe insoles should be individually fitted by an orthopedic shoemaker or podiatrist or purchased from a specialist retailer (now also online).
2. Regular inspection
• Shoe insoles should be checked regularly.checked and adjusted or replaced as needed to ensure their effectiveness.
3. Care
• Most shoe insoles can be cleaned with mild soapy water or machine washed and air dried. It is important to follow the manufacturer's instructions.
Shoe insoles are a versatile and effective way to treat various foot problems and improve overall foot health. With proper selection and fitting, they can reduce pain, improve foot function and prevent injury.
Diabetes type 2
Type 2 diabetes, also known as non-insulin-dependent diabetes mellitus or adult-onset diabetes, is a chronic disease in which the body is unable to use insulin effectively or does not produce enough insulin. Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels by promoting the transport of glucose from the blood into cells, where it is used for energy.
1. Insulin resistance
• In type 2 diabetes, the body's cells no longer respond properly to insulin. This insulin resistance means that glucose does not enter the cells effectively and accumulates in the blood.
2. Reduced insulin production
• Over time, the pancreas can no longer produce enough insulin to meet the increased demand caused by insulin resistance.
3. Genetic factors
• A family history can increase the risk of developing type 2 diabetes.
4. Overweight and obesity
• Being overweight, particularly fat accumulation in the abdominal area, increases insulin resistance and the risk of type 2 diabetes.
5. Lack of exercise
• Lack of physical activity contributes to weight gain and increases the risk of insulin resistance.
6. Unhealthy diet
• A diet rich in high-calorie, high-fat and sugary foods can contribute to the development of type 2 diabetes.
7. Age
• The risk of developing type 2 diabetes increases with age, especially after age 45.
8. Ethnicity
• People of certain ethnic groups (e.g., African Americans, Hispanics, Asian Americans, Native Americans) have a higher risk of developing type 2 diabetes.
The symptoms of type 2 diabetes often develop slowly and may be mild at first. The most common symptoms include:
• Increased thirst and frequent urination.
• Increased hunger.
• Unexplained weight loss.
• Tiredness and weakness.
• Blurred vision.
• Slow healing of wounds and infections.
• Dark patches on the skin, especially in the armpits and neck (acanthosis nigricans).
Type 2 diabetes is diagnosed through several blood tests, including:
• Fasting blood sugar test: Measures blood sugar levels after a period of fasting.
• HbA1c test: Reports the average blood sugar level over the past 2-3 months.
• Oral glucose tolerance test (OGTT): Measures blood sugar levels before and after drinking a sugary solution.
Treatment of type 2 diabetes focuses on controlling blood sugar levels to prevent complications. Key measures include:
1. Lifestyle changes
• Healthy diet: Eating a balanced diet high in vegetables, fruits, whole grains and lean proteins.
• Regular physical activity: At least 150 minutes of moderate exercise per week.
• Weight management: Losing weight can improve insulin sensitivity and lower blood sugar levels.
2. Drug therapy
• Oral antidiabetics: Various medications that increase insulin production, reduce insulin resistance, or slow the absorption of glucose in the intestine.
• Insulin therapy: Some patients require additional insulin to control blood sugar levels.
3. Blood sugar control
• Regularly monitor blood sugar levels to make sure they stay within the target range.
Uncontrolled type 2 diabetes can lead to serious complications, including:
• Cardiovascular disease (heart attack, stroke).
• Kidney damage (diabetic nephropathy).
• Nerve damage (diabetic neuropathy).
• Eye damage (diabetic retinopathy).
• Foot problems (infections, ulcers, amputations).
Preventive measures to reduce the risk of type 2 diabetes include:
• Maintaining a healthy weight.
• Regular physical activity.
• Eating a healthy diet.
• Regular health checks, especially if risk factors are present.
With timely diagnosis and appropriate treatment, type 2 diabetes can be well controlled and the quality of life of those affected can be significantly improved.

Pathophysiological classification of the diabetic foot - Neuropathic Foot
Symptoms
• Hot
• Pink
• Dry and cracked skin
• Deformities
• Insensitivity to pain
• Pulsating veins
• Swollen veins
• Swollen foot
Pathophysiological classification of the diabetic foot – Ischemic foot
Symptoms
• Cold
• Pale with elevation, cyanosis with inclination
• Thin and shiny skin
• Without deformations
• With painful sensation
• Reduced or absent pulsation
• Increased capillary refill time
• Without edema
Type 2 diabetes patients are particularly susceptible to foot problems due to circulatory disorders and nerve damage (diabetic neuropathy). It is important to take preventive measures to avoid serious complications such as infections, ulcers and amputations. Here are some tips on how type 2 diabetes patients can prevent foot problems:
Daily foot care
1. Daily inspection
• Examine your feet daily for blisters, cuts, redness, swelling or other changes. Use a mirror to check hard-to-see areas or ask for help.
2. Washing and drying
• Wash your feet daily with warm water and mild soap. Dry them thoroughly, especially between the toes, to avoid moisture and fungal infections.
3. Moisturizing
• Use a moisturizing lotion to keep skin soft and supple, but avoid applying lotion between the toes.
Foot and nail care
4. Nail care
• Trim your toenails straight and file down rough edges to prevent ingrown nails. Have nails trimmed by a podiatrist if necessary.
5. Callus treatment
• Gently remove calluses with a pumice stone after bathing, but avoid using sharp objects or chemicals.
Shoes and socks
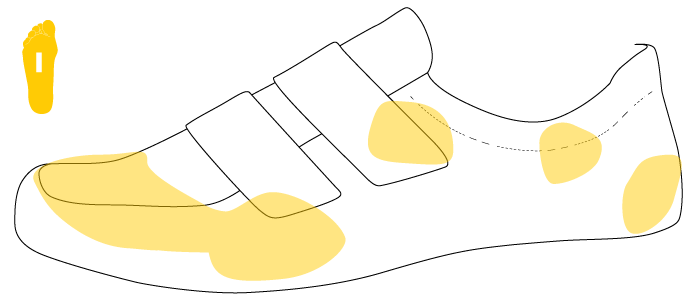
6. Appropriate shoes
• Wear well-fitting, comfortable shoes that offer enough room for your toes and do not cause pressure points. Special shoes for diabetics, for example, have no inner seam, so that sores cannot form. Avoid tight or ill-fitting shoes.
7. Shoe insoles
• Use orthopedic insoles if necessary to distribute pressure evenly and provide additional comfort.
8. Changing shoes
• Change your shoes regularly to avoid pressure points and to allow the shoes to dry.
9. Appropriate socks or stockings
• Wear clean, well-fitting socks or stockings made of breathable materials. Avoid stockings with tight elastic bands, which can restrict blood circulation. Socks specially designed for diabetics are recommended.
Protection and precautions
10. Avoiding injuries
• Never walk barefoot, especially outdoors, to avoid cuts and injuries. Always wear shoes or slippers.
11. Be careful with heat sources
• Avoid hot water bottles, heating pads or direct heat sources on the feet to prevent burns, as sensation may be impaired.
Regular check-ups and medical care
12. Regular doctor visits
• Have your feet checked regularly by a doctor or podiatrist, even if there are no visible problems.
13. Blood sugar control
• Keep your blood sugar levels well controlled to minimize the risk of nerve damage and poor circulation.
14. Treating foot problems
• Seek immediate medical attention if you notice any signs of infection, ulcers, or other problems.
Education and awareness
15. Self-management
• Learn about the importance of foot care and how to recognize signs of problems.
16. Support and education
• Attend training courses or support groups to get tips and support from other sufferers.
Through consistent care and attention, type 2 diabetes patients can significantly reduce the risk of foot problems and improve their quality of life.

Shoe construction
• 1. Reinforced
• 2. Wide opening
• 3. Adjustable velcro closure
• 4. Seamless welded connection
• 5. Inner lining with silver ions
• 6. Reinforced and extended
• 7. Insole construction with cushioning foam
• 8. Sole with "rocker" system

Height of the toe cap
• The toe cap is also 1 cm higher.
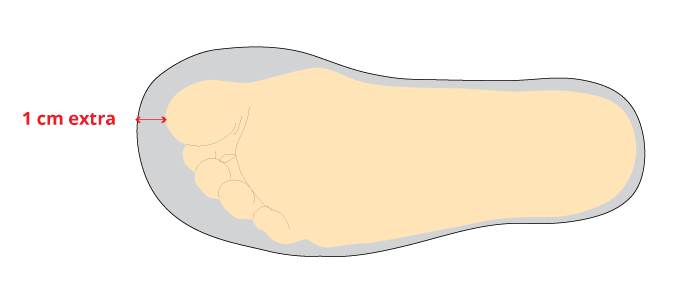
Shoe width
• Extra width on the sole of the foot with greater volume
The extra centimeter prevents the toes from hitting the shoe and increases air circulation. Diabetic feet need this extra width to avoid cramps and sores. Care must always be taken to avoid pressure points and protect swollen feet.
Toe & heel cap
• Wide, high, rounded and reinforced toe cap.
• Extended and reinforced heel cap.
Toe & heel cap allows already deformed toes to return to a more anatomically correct position. The toe cap compensates for toe deformations and protects the toes from impact. The heel cap serves to stabilize, support and prevent the ankle from twisting.
Cerebral palsy, muscular hypotonia or hypertonia, other neurological or orthopedic conditions
For the treatment of these indications, so-called DAFO orthoses are particularly well suited. A DAFO (Dynamic Ankle-Foot Orthosis) is a special type of ankle-foot orthosis (AFO) that was developed to provide dynamic stability and functionality for the foot and ankle. Unlike traditional rigid AFOs, DAFOs are more flexible and allow for better adaptation to the natural movements of the foot.
1. Dynamic Support
• DAFOs provide support without completely restricting the natural movements of the foot. They are designed to promote movement of the foot and ankle while improving stability.
2. Material and Design
• Made from thin, flexible materials that fit snugly around the foot. This allows for a better fit and comfort for the wearer.
• The orthosis can be customized to meet the child's specific needs and anatomy.
3. Improved functionality
• DAFOs help support muscle function and improve walking ability by allowing controlled movement.
• They are particularly useful in children with neurological or muscular problems who require a certain amount of mobility to develop their motor skills.
4. Indications for use
• Children with cerebral palsy who require support and stability but still want some freedom of movement.
• Children with muscular hypotonia or hypertonia who may benefit from dynamic support.
• Other neurological or orthopedic conditions requiring flexible support of the foot and ankle.
5. Function and Adaptation
• DAFOs can improve balance and correct gait by promoting better foot placement and alignment.
• Customization allows the orthosis to be tailored to the child's exact needs, increasing comfort and effectiveness.
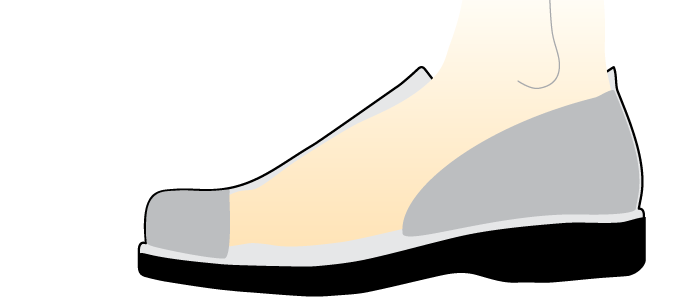
There are special shoes designed for use with orthoses, such as AFOs (Ankle-Foot Orthoses) and DAFOs (Dynamic Ankle-Foot Orthoses). These shoes provide additional support, comfort, and the room needed to comfortably accommodate the orthosis. Here are some features and types of special shoes for orthoses:
Features of special shoes for orthoses:
1. Extra width and depth
• These shoes are often wider and deeper than normal shoes to accommodate the orthosis and the foot.
2. Adjustable fasteners
• Many specialty shoes have Velcro fasteners, laces or other adjustable fasteners that make it easier to put the shoes on over the orthosis and secure them in place.
• The orthosis can be customized to meet the child's specific needs and anatomy.
3. Stable and non-slip soles
• The soles are designed to provide stability and security, which is especially important for people who wear orthoses.
4. Removable insoles
• Some models have a removable and height-adjustable insert that allows the shoe to be adapted to the orthosis and creates additional space.
• Children with muscular hypotonia or hypertonia who may benefit from dynamic support.
• Other neurological or orthopedic conditions where flexible support of the foot and ankle is necessary.
5. High-quality materials
• These shoes are made from durable, breathable materials to ensure comfort and durability.
DAFOs are an innovative solution for supporting and stabilizing the foot and ankle while promoting natural mobility. They offer individual adjustment and dynamic support that is particularly beneficial for children with neurological or muscular impairments.
Cerebral palsy, stroke, multiple sclerosis, peripheral neuropathy, muscular dystrophy, injuries
So-called AFO orthoses are particularly suitable for the treatment of these indications. An AFO (Ankle-Foot Orthosis) is an orthosis that supports and stabilizes the ankle and foot. AFOs are one of the most commonly used orthoses and are used for a variety of medical conditions and injuries.
1. Structure and Design
• AFOs are usually made of plastic, but they can also be made of metal or other materials.
• They enclose the lower leg, ankle and foot, often reaching just below the knee.
• The orthosis can be customized to fit the patient's anatomy and specific needs.
2. Aim and Benefits
• Stabilization and support: AFOs stabilize the ankle and foot, prevent unwanted movements, and improve balance.
• Correction of misalignments: They help correct foot and ankle misalignments and promote proper alignment.
• Improvement of gait: AFOs support walking by making it easier to lift the foot during the swing phase of walking and preventing dragging of the foot (so-called foot drop).
• Pain relief: By providing stabilization and support, AFOs can reduce pain caused by misalignments or instability.
3. Indications for use
• Cerebral palsy: AFOs are often used in children with cerebral palsy to control muscle spasticity and improve walking.
• Stroke: After a stroke, AFOs can help restore walking ability and improve stability.
• Multiple Sclerosis (MS): Patients with MS may benefit from AFOs to aid muscle control and facilitate walking.
• Peripheral Neuropathy: AFOs can be used to improve stability in patients with nerve damage.
• Injuries: After fractures, torn ligaments, or other injuries to the ankle or foot, AFOs can be used for stabilization and support.
• Muscular Dystrophy: When muscle weakness occurs, AFOs help support lower extremity function.
4. Types of AFOs
• Rigid (Solid AFO): Provides maximum stability and is used in cases of severe instability or severe misalignment.
• Hinged AFO: Allows limited movement in the ankle while providing support.
• Posterior Leaf Spring (PLS) AFO: A flexible variation used primarily to assist with foot elevation.
• Ground Reaction AFO (GRAFO): Used to influence knee movement and provide support to the entire lower extremity.
There are special shoes designed for use with orthoses, such as AFOs (Ankle-Foot Orthoses) and DAFOs (Dynamic Ankle-Foot Orthoses). These shoes provide extra support, comfort and the room needed to comfortably accommodate the orthosis. Here are some features and types of special shoes for orthoses:
Features of special shoes for orthoses:
1. Extra width and depth
• These shoes are often wider and deeper than regular shoes to accommodate the orthosis and the foot.
2. Adjustable closures
• Many special shoes have Velcro, laces or other adjustable closures that make it easier to put the shoes on over the orthosis and secure them in place.
• The orthosis can be customized to fit the child's specific needs and anatomy.
3. Stable and non-slip soles
• The soles are designed to provide stability and safety, which is especially important for people who wear orthotics.
4. Removable insoles
• Some models have a removableAdjustable and height-adjustable insole that allows the shoe to be adapted to the orthosis and creates additional space.
• Children with muscular hypotonia or hypertonia who may benefit from dynamic support.
• Other neurological or orthopedic conditions where flexible support of the foot and ankle is necessary.
5. High-quality materials
• These shoes are made from durable, breathable materials to ensure comfort and longevity.
An AFO is a versatile orthotic used in a variety of conditions to improve the function and mobility of the ankle and foot. It can be customized to meet the patient's specific needs and anatomy and plays an important role in lower extremity rehabilitation and support.